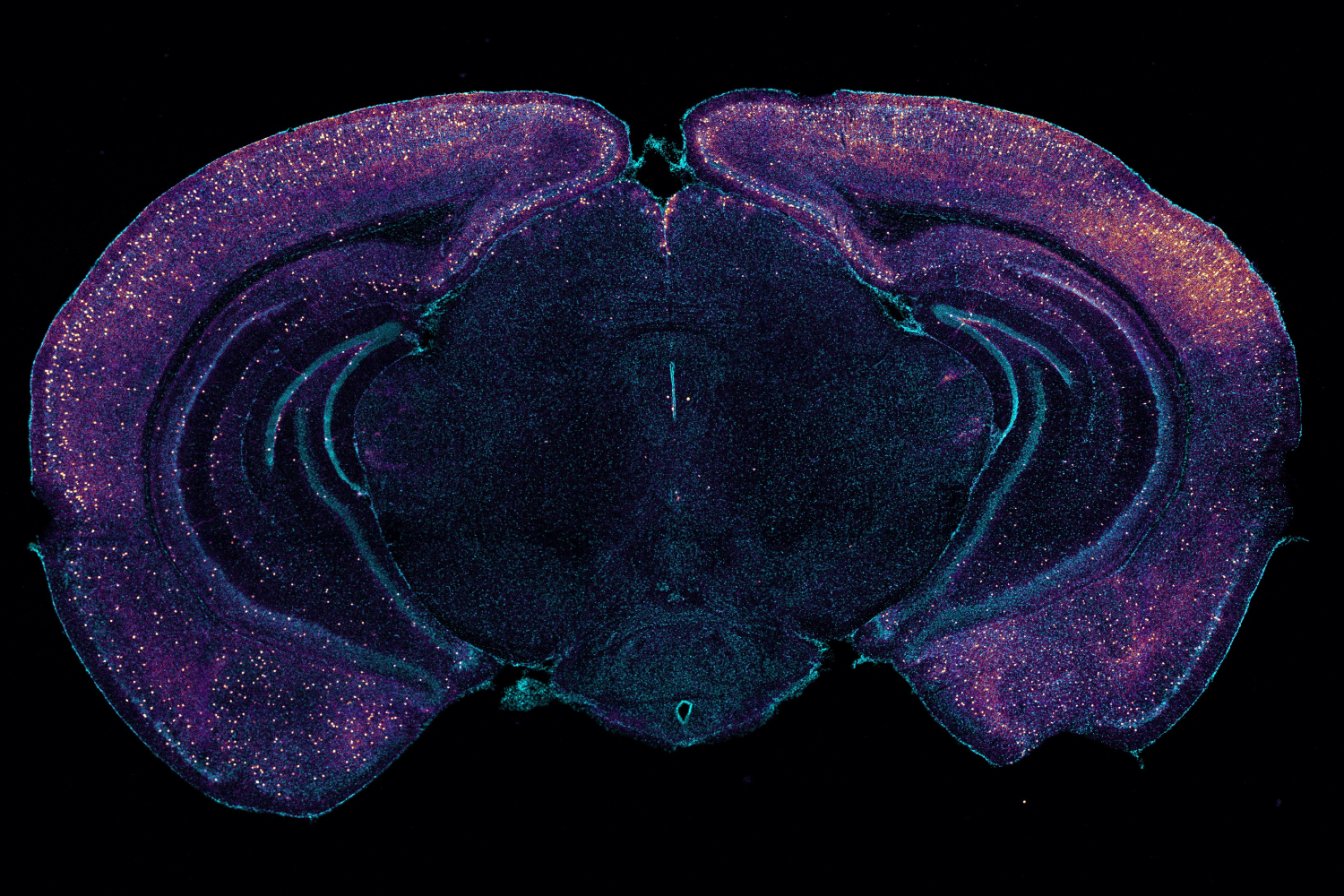
Studies at MIT and elsewhere are producing mounting evidence that light flickering and sound clicking at the gamma brain rhythm frequency of 40 hertz (Hz) can reduce Alzheimer’s disease (AD) progression and treat symptoms in human volunteers as well as lab mice. In a new open-access study in Nature using a mouse model of the disease, MIT researchers reveal a key mechanism that may contribute to these beneficial effects: clearance of amyloid proteins, a hallmark of AD pathology, via the brain’s glymphatic system, a recently discovered “plumbing” network parallel to the brain’s blood vessels.
“Ever since we published our first results in 2016, people have asked me how does it work? Why 40Hz? Why not some other frequency?” says study senior author Li-Huei Tsai, Picower Professor of Neuroscience and director of The Picower Institute for Learning and Memory of MIT and MIT’s Aging Brain Initiative. “These are indeed very important questions we have worked very hard in the lab to address.”
The new paper describes a series of experiments, led by Mitch Murdock PhD ’23 when he was a brain and cognitive sciences doctoral student at MIT, showing that when sensory gamma stimulation increases 40Hz power and synchrony in the brains of mice, that prompts a particular type of neuron to release peptides. The study results further suggest that those short protein signals then drive specific processes that promote increased amyloid clearance via the glymphatic system.
“We do not yet have a linear map of the exact sequence of events that occurs,” says Murdock, who was jointly supervised by Tsai and co-author and collaborator Ed Boyden, Y. Eva Tan Professor of Neurotechnology at MIT, a member of the McGovern Institute for Brain Research and an affiliate member of the Picower Institute. “But the findings in our experiments support this clearance pathway through the major glymphatic routes.”
How sensory gamma rhythm stimulation clears amyloid in Alzheimer’s mice
Video: The Picower Institute
From gamma to glymphatics
Because prior research has shown that the glymphatic system is a key conduit for brain waste clearance and may be regulated by brain rhythms, Tsai and Murdock’s team hypothesized that it might help explain the lab’s prior observations that gamma sensory stimulation reduces amyloid levels in Alzheimer’s model mice.
Working with “5XFAD” mice, which genentically model Alzheimer’s, Murdock and co-authors first replicated the lab’s prior results that 40Hz sensory stimulation increases 40Hz neuronal activity in the brain and reduces amyloid levels. Then they set out to measure whether there was any correlated change in the fluids that flow through the glymphatic system to carry away wastes. Indeed, they measured increases in cerebrospinal fluid in the brain tissue of mice treated with sensory gamma stimulation compared to untreated controls. They also measured an increase in the rate of interstitial fluid leaving the brain. Moreover, in the gamma-treated mice he measured increased diameter of the lymphatic vessels that drain away the fluids and measured increased accumulation of amyloid in cervical lymph nodes, which is the drainage site for that flow.
To investigate how this increased fluid flow might be happening, the team focused on the aquaporin 4 (AQP4) water channel of astrocyte cells, which enables the cells to facilitate glymphatic fluid exchange. When they blocked APQ4 function with a chemical, that prevented sensory gamma stimulation from reducing amyloid levels and prevented it from improving mouse learning and memory. And when, as an added test, they used a genetic technique for disrupting AQP4, that also interfered with gamma-driven amyloid clearance.
In addition to the fluid exchange promoted by APQ4 activity in astrocytes, another mechanism by which gamma waves promote glymphatic flow is by increasing the pulsation of neighboring blood vessels. Several measurements showed stronger arterial pulsatility in mice subjected to sensory gamma stimulation compared to untreated controls.
One of the best new techniques for tracking how a condition, such as sensory gamma stimulation, affects different cell types is to sequence their RNA to track changes in how they express their genes. Using this method, Tsai and Murdock’s team saw that gamma sensory stimulation indeed promoted changes consistent with increased astrocyte AQP4 activity.
Prompted by peptides
The RNA sequencing data also revealed that upon gamma sensory stimulation a subset of neurons, called “interneurons,” experienced a notable uptick in the production of several peptides. This was not surprising in the sense that peptide release is known to be dependent on brain rhythm frequencies, but it was still notable because one peptide in particular, VIP, is associated with Alzheimer’s-fighting benefits and helps to regulate vascular cells, blood flow, and glymphatic clearance.
Seizing on this intriguing result, the team ran tests that revealed increased VIP in the brains of gamma-treated mice. The researchers also used a sensor of peptide release and observed that sensory gamma stimulation resulted in an increase in peptide release from VIP-expressing interneurons.
But did this gamma-stimulated peptide release mediate the glymphatic clearance of amyloid? To find out, the team ran another experiment: They chemically shut down the VIP neurons. When they did so, and then exposed mice to sensory gamma stimulation, they found that there was no longer an increase in arterial pulsatility and there was no more gamma-stimulated amyloid clearance.
“We think that many neuropeptides are involved,” Murdock says. Tsai added that a major new direction for the lab’s research will be determining what other peptides or other molecular factors may be driven by sensory gamma stimulation.
Tsai and Murdock add that while this paper focuses on what is likely an important mechanism — glymphatic clearance of amyloid — by which sensory gamma stimulation helps the brain, it’s probably not the only underlying mechanism that matters. The clearance effects shown in this study occurred rather rapidly, but in lab experiments and clinical studies weeks or months of chronic sensory gamma stimulation have been needed to have sustained effects on cognition.
With each new study, however, scientists learn more about how sensory stimulation of brain rhythms may help treat neurological disorders.
In addition to Tsai, Murdock, and Boyden, the paper’s other authors are Cheng-Yi Yang, Na Sun, Ping-Chieh Pao, Cristina Blanco-Duque, Martin C. Kahn, Nicolas S. Lavoie, Matheus B. Victor, Md Rezaul Islam, Fabiola Galiana, Noelle Leary, Sidney Wang, Adele Bubnys, Emily Ma, Leyla A. Akay, TaeHyun Kim, Madison Sneve, Yong Qian, Cuixin Lai, Michelle M. McCarthy, Nancy Kopell, Manolis Kellis, and Kiryl D. Piatkevich.
Support for the study came from Robert A. and Renee E. Belfer, the Halis Family Foundation, Eduardo Eurnekian, the Dolby family, Barbara J. Weedon, Henry E. Singleton, the Hubolow family, the Ko Hahn family, Carol and Gene Ludwig Family Foundation, Lester A. Gimpelson, Lawrence and Debra Hilibrand, Glenda and Donald Mattes, Kathleen and Miguel Octavio, David B. Emmes, the Marc Haas Foundation, Thomas Stocky and Avni Shah, the JPB Foundation, the Picower Institute, and the National Institutes of Health.